Introduction
Climate change is one of the most urgent health threats of the 21st century. It drives environmental shifts that directly harm human health. Occurrences of vector-borne diseases are rising rapidly and account for many newly emerging infectious diseases (Swei et al., 2020). Vector-borne diseases are infections transmitted by blood-feeding insects such as mosquitoes, ticks, and flies. Common examples include Malaria, Dengue, Chikungunya, and Leishmania (Jwanse1sis et al., 2021). These diseases thrive in warm, humid environments where vectors can breed and survive. Mosquitoes are among the world’s most widespread and deadliest disease vectors, transmitting serious illnesses like Malaria, Dengue, Zika, and Yellow Fever across many regions (Bakri and Jadkarim, 2024). As this article focuses on various diseases, there are several images that contain injury content, which may be graphic for some.
Climate change drives disease spread by warming temperatures and shifting rainfall. Over 90% of this impact comes from human-induced greenhouse gas emissions. As a result, vector-borne diseases now appear in areas once unaffected (Biswas, 2022). Without urgent action, the disease burden will rise and affect millions. Addressing this crisis is vital for the continent’s health and economic future.
The THRIVE Framework offers a solution. It promotes Systems Thinking, Strong Sustainability, and long-term adaptation. Its core principle, thrivability, focuses on solutions that are effective now and regenerative over time. By applying this model, African nations can build resilience and respond to climate-driven health risks more effectively.
How GLOBAL Warming, Rainfall Shifts, and Weak Systems Fuel Vector-Borne DISEASES
Climate change reshapes the landscape of global health, particularly in regards to the spread of vector-borne diseases. These diseases, transmitted by mosquitoes, ticks, and other vectors, are highly sensitive to environmental changes such as temperature, rainfall, and humidity. As the planet warms, these factors become increasingly unpredictable, making it harder to control and predict outbreaks.
1. Rising Temperatures and Changing Rainfall Patterns
Climate change directly affects the spread of vector-borne diseases. Rapid climate changes have increased parasites, pathogens, and vector populations, threatening global health and the environment (Yadav and Upadhyay, 2023). These rising temperatures include an increase of 0.1-0.3°C per decade across Africa. Warmer temperatures extend mosquito and tick breeding seasons, allowing them to thrive in previously colder areas (Thomson et al., 2018). This expansion spreads diseases like Malaria, Dengue, and Lyme disease to new regions.
Shifting rainfall patterns also create new breeding sites for mosquitoes and ticks. In areas like the Sahel region and East Africa, erratic rains disrupt seasonal vector distribution (Palmer et al., 2023). Heavy rains foster standing water, perfect for mosquito larvae. In contrast, droughts reduce water sources, affecting both vectors and local communities.
2. The Role of Climate Variability and ENSO
The El Niño Southern Oscillation (ENSO) is another critical driver influencing the climate in Africa (Ranaweera and Kamae, 2024). This phenomenon affects temperature and rainfall patterns across the continent, leading to increased climatic extremes. The study conducted across Western, Eastern, and Southern Africa revealed that year-to-year climate variations, often linked to ENSO events, have a significant impact on the spread and intensity of vector-borne diseases. For example, during El Niño years, changes in rainfall can create optimal conditions for disease transmission, while in drought years, lower vector survival rates may reduce disease risks (Thomson et al., 2018).
3. Using Climate Data for Early Warning Systems
Understanding climate variations is key to managing the risks posed by vector-borne diseases. The research highlights the importance of integrating climate data into public health strategies, particularly in Africa, where the burden of these diseases is high. Seasonal climate forecasts and observed data are valuable tools for early warning systems, allowing health authorities to predict outbreaks and respond more effectively. However, the accuracy of these forecasts can vary by region and season, making it crucial to tailor responses based on specific local conditions (Connor & Mantilla, n.d.).
4. Expanding Range of Mosquitoes and Ticks in Africa
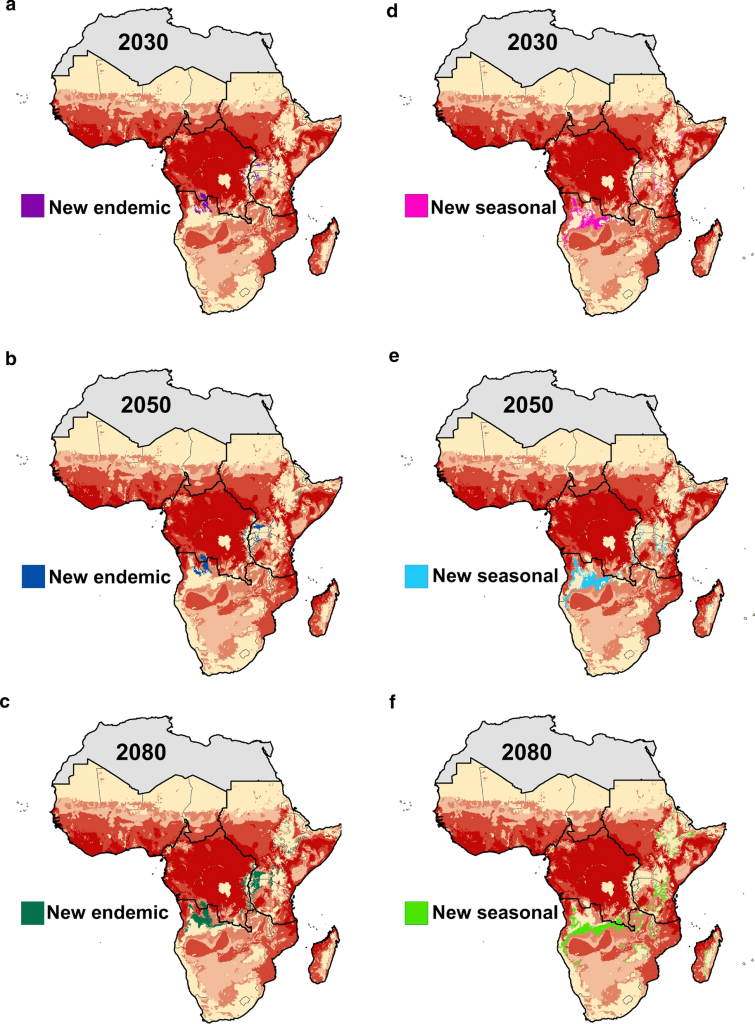
Climate change is significantly expanding the range of mosquitoes and ticks across Africa, directly increasing the spread of vector-borne diseases like malaria and dengue. Rising temperatures, shifting rainfall patterns, and increased humidity are key drivers of this shift, with studies predicting higher disease prevalence in regions previously unaffected. This shift not only impacts public health but also threatens ecosystems, as new areas become vulnerable to disease outbreaks (Lehmann et al., 2023).
In Africa, climate change increases disease spread in vulnerable areas with weak health systems. Moreover, extreme weather, displacement, and poor infrastructure worsen control efforts. As a result, vector-borne disease burdens grow. Therefore, urgent action is needed to protect public health and build resilience.
Mosquitoes are the deadliest vector of disease, responsible for spreading Zika, Dengue fever, West Nile fever, Chikungunya, Yellow Fever, and Malaria.
Source: ENSURE IAS
Key Vector-Borne DISEASES Affected by Climate Change in Africa
1. Malaria
Malaria continues to pose a significant health threat in Sub-Saharan Africa, which carries the highest global burden. Each year, over 200 million cases and 400,000 deaths occur, mainly among children under five. Moreover, issues like poverty, weak health systems, and insufficient political commitment complicate control efforts. In addition, climate change and rapid population growth accelerate mosquito breeding and disease transmission (Kogan, 2020). Climate change will significantly shift malaria transmission zones, exposing over 75 million more people to endemic risk in Eastern and Southern Africa by 2080 (Ryan et al., 2023).
Source: Malaria Journal
2. Dengue and Chikungunya
Aedes Mosquitoes spread both Dengue and Chikungunya. Dengue fever is a mosquito-borne illness caused by four related viruses, similar to those responsible for West Nile Fever and Yellow Fever. Every year, about 400 million people are infected globally, with 96 million showing symptoms. High-risk regions include Southeast Asia, the Indian subcontinent, Africa, and Latin America. Aedes Mosquitoes spread the virus by biting infected individuals and then healthy ones (Jwanse1sis et al., 2021). Dengue outbreaks have emerged in Africa, with Burkina Faso reporting 214 deaths in 2023, mostly in major cities. Notably, between 9th–15th October 2023, 48 deaths occurred as Dengue cases spiked alongside a Chikungunya outbreak (George et al., 2024).
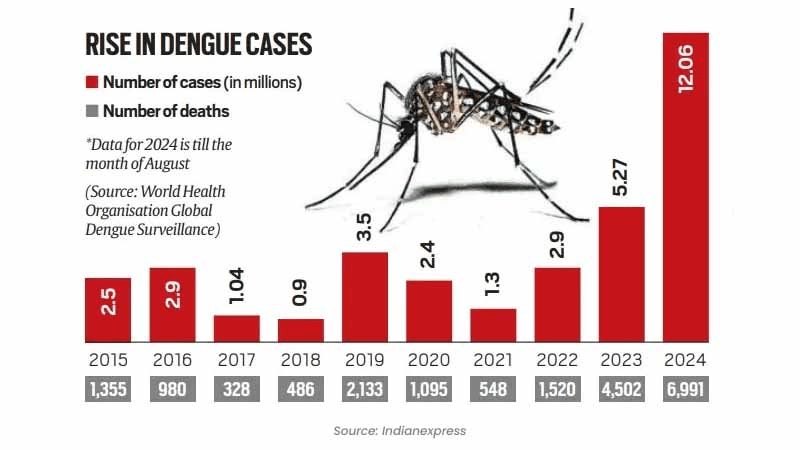
Source: The Wellness Corner
3. Schistosomiasis
Schistosomiasis is a parasitic infection spread through freshwater snails, which affects impoverished populations and livestock in tropical regions. Although control efforts have made progress, it continues to prevail in much of Sub-Saharan Africa. As a result, around 800 million people remain at risk (Aula et al., 2021). Changing water levels caused by erratic rainfall and flooding alter the habitats of these snails, making it easier for people to contract the disease.
Schistosomiasis remains a neglected tropical vector-borne disease, particularly affecting Sub-Saharan Africa. Consequently, millions remain at high risk. Moreover, climate change worsens the situation by altering rainfall and increasing temperatures. As a result, these changes expand snail habitats and raise infection rates (Adekiya et al., 2020). Specifically, Bulinus Truncatus, a key vector, thrives in new regions owing to warming climates. Therefore, areas like Central Africa and Southern Europe now face increased transmission risks (Deure et al., 2024).
4. Leishmaniasis
Leishmaniasis, a vector-borne parasitic disease transmitted by sandflies, is increasingly affecting regions in North and East Africa owing to climate change and environmental disruption. As temperatures rise and ecosystems shift, conditions become more favorable for the survival and spread of sandfly populations. In particular, land-use changes such as deforestation, urbanisation, and desertification are expanding sandfly habitats, leading to a surge in reported cases (Jones & Welburn, 2021). For instance, in Morocco, Leishmania Tropica and its vector Phlebotomus Sergenti are expected to expand their range under future climate scenarios, significantly increasing the risk of Anthroponotic Cutaneous Leishmaniasis (ACL) (Daoudi et al., 2022). These developments highlight an urgent need for climate-adaptive disease control strategies, including improved vector surveillance, targeted interventions, and further research into L. Tropica reservoirs. Without timely and effective responses, Leishmaniasis may continue to spread into previously unaffected areas, posing a severe threat to public health across the region.
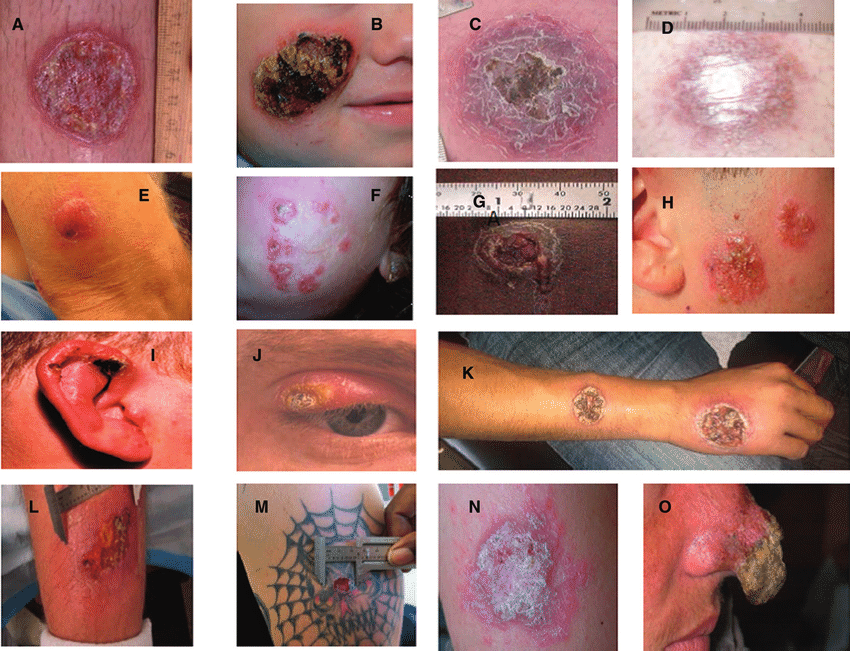
Source: ResearchGate
Vulnerable Populations and Regions in Africa
The impact of climate change on vector-borne diseases is most severe in:
- Sub-Saharan Africa: This region, already facing high poverty rates, is seeing increased desertification and water scarcity, which heightens disease risk.
- East African Highlands: Rising temperatures are allowing malaria to spread to higher altitudes, where it was once uncommon.
- Urban slums: Poor infrastructure and sanitation turn informal settlements in African cities into hotspots for disease transmission.
Children, pregnant individuals, and those with weakened immune systems are especially vulnerable. They are more likely to suffer severe complications from diseases like Malaria and Dengue. The interplay between poverty, poor health infrastructure, and climate change exacerbates these risks, creating a vicious cycle of vulnerability.
Strategies for Mitigating the Impact of Climate Change on neglected tropical diseases
1. Integrated Surveillance Systems
Using data on climate and weather patterns alongside health data can help predict disease outbreaks (Indhumathi & Kumar, 2021). Early warning systems that integrate climate forecasts with health trends will allow public health officials to respond more effectively.
2. Innovative Vector Control
Innovations in vector control, such as genetically modified mosquitoes or eco-friendly insecticides, can play a major role in curbing the spread of diseases (Tyagi et al., 2021). These solutions align with THRIVE Project’s emphasis on Values-Based Innovation, which seeks to balance human health with environmental sustainability.
3. Community Engagement
Involving communities in disease prevention is crucial. Educating people on how to reduce vector breeding sites such as cleaning standing water and using mosquito nets can significantly reduce transmission. Local solutions, driven by community knowledge, are often the most effective and sustainable.
4. Infrastructure Development
Improving water and sanitation systems can prevent vector-borne diseases like Malaria and Schistosomiasis by eliminating breeding grounds (Velleman et al., 2023). Building climate-resilient infrastructure also ensures that communities are better prepared for future climate impacts, making them more resilient to health risks.
How Do we Stop Vector-borne Diseases?
The rising impact of climate change on vector-borne neglected tropical diseases in Africa is undeniable. However, with the right strategies, policies, and community-driven efforts, we can mitigate these risks and build a more resilient future. By adopting a systemic and integrated approach, we can ensure that our responses are not only effective but also regenerative, sustainable, and equitable.
To this end, governments, international organisations, and local communities can:
- Invest in early warning systems that integrate climate data and health trends to predict outbreaks.
- Support local innovation in vector control and disease prevention methods.
- Adopt climate-resilient health policies that prepare populations for the health challenges of tomorrow.
By acting now, we can reduce the burden of vector-borne diseases and create a thriving, healthier future for all.
How does this solve the issues our world faces?
This topic strongly aligns with several of the UN’s Sustainable Development Goals (SDGs), particularly those focused on health, climate action, poverty reduction, and environmental sustainability. Climate change intensifies the spread of vector-borne neglected tropical diseases (NTDs), posing serious risks to human health and public health systems. Addressing diseases like Malaria, Dengue, and Schistosomiasis supports SDG3: Good Health and Well-Being by reducing illness and premature death. It also helps SDG6: Clean Water and Sanitation by promoting better hygiene and reducing breeding sites for vectors. Improved sanitation systems lower disease incidence and strengthen community resilience.
Moreover, tackling NTDs supports broader climate and development goals. For example, SDG13: Climate Action is advanced through health system adaptation and disease surveillance. By reducing disease burdens, we also progress on SDG1: No Poverty and SDG10: Reduced Inequalities, protecting the most vulnerable populations. Investments in SDG9: Innovation and Infrastructure enable climate-smart health systems and technologies. Additionally, SDG15: Life on Land is supported by protecting ecosystems that regulate vector habitats and reduce transmission risks. Together, these efforts build healthier, more equitable, and climate-resilient communities.
the Thrive Framework: How it can help reduce vector-borne diseases
The THRIVE Framework offers a comprehensive and adaptive approach to tackling the combined challenges of climate change and vector-borne diseases in Africa. The Systemic Holistic Model stresses the interconnectedness of environmental, health, and social systems. As climate change disrupts ecosystems, vectors like mosquitoes and ticks expand their range, spreading diseases such as Malaria and Dengue to new areas. The framework advocates for integrated solutions that combine climate adaptation strategies with health policies, community resilience, and sustainable practices.
The Finite Resources element recognises the limited resources available in many African regions and emphasises prioritising interventions that have the highest impact. Targeted actions such as climate monitoring, vector control, and public health initiatives help make the most of these scarce resources and minimise the spread of diseases.
The THRIVE Framework integrates Science-Based Targets to set measurable goals for reducing disease transmission and addressing climate change impacts. It also uses Context-Based Metrics to tailor interventions to local climate, health systems, and socio-economic conditions. By aligning strategies with regional needs, THRIVE Framework maximises resources, enhances resilience, and improves health outcomes, particularly in tackling climate-driven vector-borne diseases across Africa.
You can follow us on social media platforms such as LinkedIn, Instagram, and Facebook. Additionally, you could subscribe to our YouTube channel, and listen to our podcasts You can also sign up for our newsletter, stay up to date with our articles, attend our free webinars, or even join us as a volunteer to make an even greater impact on the world.