Whilst the COVID-19 pandemic has swept the globe, another silent pandemic reveals the need to enforce a healthy lifestyle – antibiotic resistance. In fact, the World Health Organisation (WHO) labels antimicrobial resistance (AMR) as one of the top 10 global health concerns for humankind. So the real question is, how is antibiotic resistance connected to Sustainable Development Goals (SDGs) and what can we do to minimise this silent pandemic? Let’s take a look at the link between antibiotic resistance and the need to enforce SDGs 3 and 12 for a healthier lifestyle.
Before looking at AMR, let us understand what are antibiotics.
Antibiotics, the super innovation that treats all dangerous infections and life-threatening diseases, are something we are familiar with. And we owe it to Alexander Fleming who discovered penicillin accidentally. It is supposed that when he returned from his holiday, he noticed a fungus that had contaminated his culture plate of Staphylococcus bacteria, which he had left uncovered. This fungus which is called Penicillium notatum had created some bacteria-free zones, where it grew on that plate. Fleming found this very strange and isolated that species and grew it in a pure culture medium.
How do antibiotics work?
Antibiotics are used for those infections caused by bacteria and come under the classification of medicines called antimicrobials. The way antibiotics work is by damaging the bacteria so that the body’s immunity can fight the bacteria out of the system easily.
However, overusing them can cause something new in the medical world known as antibiotic resistance.
What Is Antimicrobial Resistance?
Now, what would happen if the antibiotics were used so often by a patient? The bacteria will ultimately evolve against that antibiotic and finally get to a stage where it can resist its effect. And the result is what the world today sees as antibiotic resistance. This serious problem simply means that the dosage of the prescribed antibiotics will not be enough to treat the bacterial infection growing inside your body.
How does antibiotic resistance happen?
Antibiotic resistance happens when you take antibiotics when you do not need them, resort to incomplete dosages, or take those prescribed for someone else. The bacteria acquire some form of resistance to that antibiotic medicine and become what is commonly called a “superbug.”
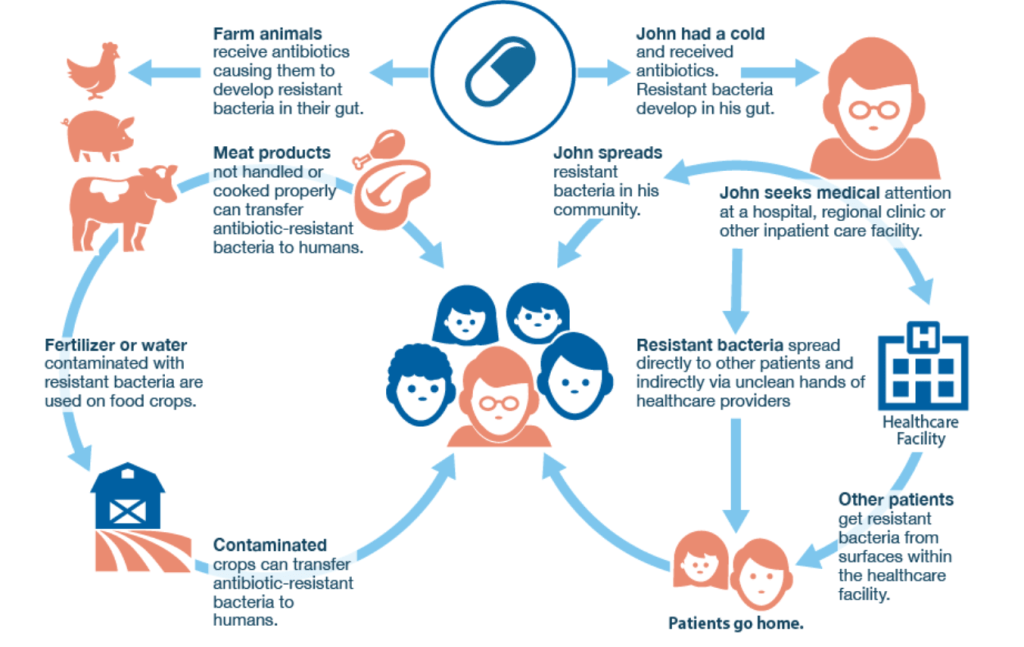
Figure 1: The spreading of antimicrobial resistance (Source: Antiobiotic Store online)
What are the dangers of AMR?
Antimicrobial resistance is a reality in many countries including Australia. Among the 29 EU countries, Australia stands as the eighth highest user of antibiotics. AMR is threatening the types of medicine available to treat various infections like tuberculosis, HIV, leprosy, malaria, typhoid, and even gonorrhea. These commonly known diseases that have had reliable cures are suddenly becoming difficult to treat in certain patients because of AMR. And according to World Health Organisation (WHO), AMR causes about 4.95 million cases in 2019 alone.
What causes Antimicrobial Resistance?
We all know of the most common factor for developing an AMR. It is through over-abusing our bodies by giving it regular doses of antibiotics even when not prescribed or not required. Another shocking factor is the overuse of antibiotics in raising our livestock for food. Raising healthy, good quality, and safe animals for food is a requirement for farmers, which propels the use of antibiotics if infections persist. AMR occurs when the bacteria is resistant to the drugs and is not killed, and the drugs prove ineffective.
The Connection between AMR and Climate Change
Now, research has also proved that climate change also impacts AMR. The rate of infection associated with the increase in temperature is also seen. Few antibiotic-susceptible infections will occur during the cooler winter months. Global warming also means warmer climates and more storms, resulting in increased precipitation and eventually floods. Flooding results in displacement of people and refugees and overcrowding, which ultimately means spreading of infection among people. These will result in the widespread of waterborne diseases. The overuse of fertiliser, specially Nitrogen fertilisers, increases antibiotic resistance, and therefore, nitrogen fertilisers pollution of floodwater during severe flooding will also lead to an increase in antibiotic resistance. Eutrophication, a phenomenon that occurs when the waterbody has a higher nitrogen content and causes an overgrowth of algae, can also increase the risk of antibiotic resistance.
Investigating National Initiatives
According to a study done by the WHO, only 50% of the world’s countries have an “AMR multisectoral coordination mechanism” to prioritise action plans. Well, In 2020, the government of Australia launched a strategy to protect the health of humans and the environment through their 20-year National Antimicrobial Resistance Strategy.
This shows that a lot needs to be done, and public awareness about this is required more than ever. It could also be certain that people do not know that an overdose is going to harm them in the long run.
How to prevent AMR?
- Reduce your dependence on meat as this will reduce your intake of these AMR strains.
- Be healthy, so that your immunity will be at its best function to treat you rather than be dependent on antibiotics.
- Practise hygienic handwashing practices, and strong infection-control practices help reduce the risk of infection in the first place.
Can a Healthy Lifestyle Affect Antimicrobial Resistance?
By now, it is quite clear that maintaining a healthy lifestyle will help you prevent infections in the first place. This also means lesser exposure to antibiotics and lesser chances of developing AMR. A healthy lifestyle also translates to a powerful immune system, which will support your recovery if you catch any bug, and that also means you would not be prescribed any antibiotics by the doctor.
What people do not realise is that antibiotics disrupt the gut microbiome, which can be then made up by having prebiotic and probiotic foods. A healthy lifestyle and diet will strengthen your gut bacteria and keep you healthy from within.
SDG 3 (healthy lifestyle) and antibiotic resistance are more connected than we think. According to the WHO, the amount of antibiotics found in food-producing animals associates itself with the development of antimicrobial-resistant bacteria in extreme animal production conditions. In other words, food-producing animals and the antibiotics used to treat their health connect to the transmission of antibiotic medicines between humans and animals. Examples of human-to-animal transmissions are via direct contact or through animal product consumption.
Therefore, SDG 3 and the reduction in meat consumption play a key role in minimising the transmission of antimicrobial bacteria in humans. Fortunately, food choices are something that we can control. For instance, every time you include more vegetables in your meals, you decrease the dependence on meat consumption. So reducing meat consumption is not only the key to beating this pandemic but the key to a healthy lifestyle.
Secondly, SDG 12 (responsible consumption and production) and antibiotic use are significantly linked. For instance, according to Medpage Today, antibiotic overuse is the driving force of antibiotic resistance. Thus, over-prescribed antibiotics and enforcing SDG 12 may help to develop sustainable prescription use. In addition, patients not taking their prescribed antibiotic medication are the silent force behind antibiotic resistance. Similarly, the factors mentioned have an effect on not only our well-being but the environment—here’s why.
How Do the SDGs Influence Antimicrobial Resistance?
Focus on the importance of SDGs that promote health and well-being and why these SDGs are important in the context of AMR.
Firstly, you might not think avoiding prescription meds contributes to the environment, but it does. By avoiding taking prescribed medication, you may increase your number of doctor visits! Hence, by driving to the doctor, you’re increasing your carbon footprint and car exposure. Also, we rely on plant biodiversity for traditional medicine and to aid us in pharmaceutical development. Thus, overconsuming non-prescription drugs contributes to the issue of sustainable plant development. Therefore, the simplest way to avoid developing further antibiotic resistance and to live a healthier lifestyle is by taking and not sharing your prescribed meds!
Doctors, Pay Attention to Overprescribing Antibiotics!
Over-prescribing medication is not only bad for the environment but also the biggest factor in antibiotic resistance. Think about it. Wouldn’t the world be a better place if people took the correct doses of medication? By enforcing SDG 12 in the medical industry, doctors have the power to control their contribution to medical waste. Therefore, over-prescribing drugs contributes to the need to enforce waste management on pill bottles. But what can the average person do? If your doctor overprescribed medicine to you, first see where you can dispose of extra prescribed drugs. In addition, reuse or recycle your prescription pill containers. Contact your local community recycling center or pharmacy for pill bottle recycling rules and regulations. By doing your part, you can feel happy, knowing that you’re contributing not only to SDG 12 but to a healthier lifestyle for the environment.
By 2050, researchers predict, antibiotic resistance will globally cause 10 million deaths each year. Antibiotic resistance has already knocked on our door. The antibiotic resistance pandemic is already here and will not be backing down anytime soon. Hence, it’s up to all of us to take the following measures to ensure that our planet and people live nothing but a healthy lifestyle.
A Thrivable Framework
Tired of wanting to make a difference but don’t know how to? Join our THRIVE tribe! We’re always looking for people who want to make a difference, so join our community and take part in the fight for a better world! To read more about sustainable development and how to battle climate change, you can tune in to our website and the following links:
- THRIVE Framework and Platform
- THRIVE Framework Playlist on YouTube
- THRIVE Framework & The Systemic Holistic Model
- THRIVE Framework Documents
- THRIVE Framework Glossary
- THRIVE Framework Brochure
Conclusion
Stay aware of this threat, and educate your family. Next time you have a common cold or small infection, let your body heal itself, and eat immunity-boosting foods that will help your body deal with infections so that when the time comes for a life-threatening disease, the antibiotic will work in your body.