Introduction
Family planning has long been considered a woman’s responsibility (Christin-Maitre, 2013), leaving men with limited options beyond condoms and vasectomies. However, shifting societal norms and advancements in medical research have reignited discussions about male birth control. More men are expressing an interest in playing an active role in family planning (Martins and Boraas, 2023). Expanding options for male contraception not only enhances reproductive choices but also promotes gender equality and reduces unintended pregnancies.
A Brief History of Male Contraceptives
According to Drucker (2020), societies have been exploring ways to prevent pregnancy for centuries. Ancient civilisations used rudimentary methods, including herbal remedies and mechanical barriers. The 20th century brought significant advancements, particularly for women, with the introduction of oral contraceptives and intrauterine devices (Cheung et al., 2021). Male contraception, however, remained largely unchanged, with condoms and vasectomies being the primary options. Research into hormonal and non-hormonal alternatives has progressed, yet male birth control is still not widely available (Amory, 2019).
Why does Male Family planning Matter?
Unintended pregnancies contribute to economic strain, health complications, and social challenges (Yazdkhasti et al., 2015). Shared responsibility in contraception can ease this burden. Ensuring men’s engagement in reproductive health decision-making can lower the risk of unintended pregnancies and related health complications by addressing many barriers (Kabagenyi et al., 2014). Barriers include partner opposition, reproductive coercion, and myths about contraception stemming from cultural norms and unequal power relations. Additionally, male birth control can help lower sexually transmitted infection rates and foster more equitable relationships (Nkonde et al., 2023).
Studies have shown that family planning has numerous benefits, including reducing maternal, child, and infant mortality, protecting against unplanned pregnancies, and supporting sustainable socioeconomic development. It is estimated that proper family planning could avert up to 42% of maternal mortality (Anbesu et al., 2022).
Types of male contraceptive choices
Male contraceptive methods: physical, hormonal, and surgical.
Each has its own mechanism, effectiveness, and potential for reversibility.
Physical Methods
Condoms: The most commonly used male contraceptive. They are affordable, widely available, and effective in preventing both pregnancy and sexually transmitted infections (STIs) (BANSAL, 2024).
Withdrawal Method: This involves the male partner pulling out before ejaculation to prevent sperm from entering the vagina. Although it is frequently practiced, it is unreliable since sperm can be present in pre-ejaculatory fluid, increasing the risk of pregnancy.
Heat-Based Methods: Recent innovations involve external heat application to temporarily suppress sperm production. Applying heat to the testes temporarily reduces sperm production by disrupting spermatogenesis, as sperm cells require a lower temperature to develop properly. Methods such as heated underwear or ultrasound exposure are under investigation. Although promising, further research is needed to ensure long-term safety and effectiveness (Joubert et al., 2022).

Source: Freepik
Hormonal Methods
- Injectables: These injections contain testosterone and progestin, which signal the brain to reduce the follicle-stimulating hormone (FSH) and luteinising hormone (LH) production. This suppression prevents the testes from producing sufficient sperm while maintaining male hormone balance (Page et al., 2022).
- Hormonal Gels: Applied daily to the shoulders, these gels deliver synthetic testosterone, which suppresses natural testosterone production in the testes. As a result, sperm production drops significantly while maintaining necessary testosterone levels in the bloodstream (Sitruk-Ware et al., 2025).
- Implants: Small rods inserted under the skin slowly release synthetic hormones that suppress sperm production. They work similarly to hormonal injections but provide long-term contraceptive effects (without requiring frequent administration (Kroopnick et al.,2024).

Source: Drug Discovery
Non-Hormonal Methods
- RISUG (Reversible Inhibition of Sperm Under Guidance): A polymer injected into the vas deferens creates a gel-like barrier that disables sperm as they pass through. A second injection dissolves the polymer, restoring fertility when desired (Lohiya et al., 2022). ‘Vaso-occlusive methods are the only nonhormonal male contraceptive method to reach clinical trials in men’ (Abbe et al., 2020).
- Vasalgel: Functioning similarly to RISUG, this gel blocks sperm movement in the vas deferens. However, human trials are still needed to confirm its long-term effectiveness and reversibility (Jimenez et al., 2023).
- Sperm Motility Inhibitors: These experimental drugs target sperm movement rather than production. By preventing sperm from swimming efficiently, they reduce the likelihood of fertilisation (Wen et al., 2021).
Surgical Methods
- Vasectomy: A permanent surgical procedure where the vas deferens is cut and sealed, preventing sperm from mixing with semen. While highly effective, reversal is difficult and not always successful (Schulz et al., 2023).
- Reversible Vasectomy: Emerging techniques, such as clip-based procedures and Vasalgel, aim to block sperm transport temporarily. Unlike traditional vasectomies, these methods may offer an option to restore fertility when needed (Nirooman & Mirzaii-Dizgah, 2020).
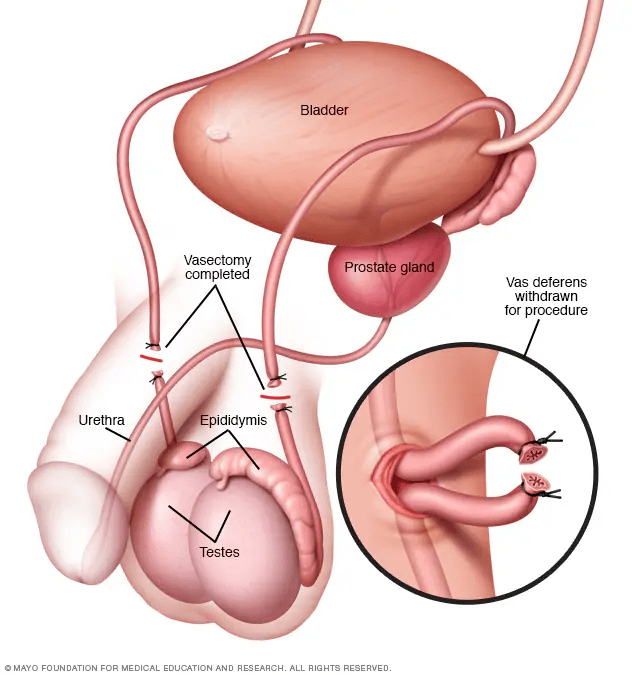
Source: Mayo Clinic
How Effective Are Male Birth Control Methods?
The success of male contraceptives depends on the method used. Condoms prevent pregnancy in 98% of cases with perfect use but drop to 87% with typical use (Thirumalai and Page, 2020). The withdrawal method remains common but fails about 20% of the time. Heat-based methods, which temporarily suppress sperm production, show promise, but researchers need more data on their long-term reliability. Hormonal methods like injectables, gels, and implants achieve over 95% effectiveness by reducing sperm count. However, these options require strict adherence, and some men experience side effects. Non-hormonal methods, such as RISUG and Vasalgel, block sperm transport and show nearly 100% effectiveness. Vasectomy remains the most reliable option, preventing pregnancy in over 99% of cases, though its permanence limits its appeal.
Are These Methods Reversible?
Fertility recovery varies by contraceptive type. Condoms and withdrawal allow immediate restoration, while heat-based methods temporarily suppress sperm and take weeks or months to reverse. Hormonal methods take longer, with injectables requiring months and implants up to a year for sperm production to normalise. Non-hormonal methods like RISUG and Vasalgel are designed for reversibility. A dissolving injection can restore sperm flow, but more studies are needed. Vasectomies remain the least reversible, with reversal procedures being expensive and not always successful (Andino et al., 2021). Researchers are testing clip-based vasectomy techniques and vas-occlusive gels as temporary alternatives, though they require further evaluation.
The Science Behind Male Birth Control
Scientists are developing safe and effective male contraceptives through extensive research. They focus on disrupting sperm production, motility, or transport (Melanie and Eberhard, 2009). Non-hormonal methods like RISUG inject a polymer into the vas deferens to block sperm flow, showing nearly 100% effectiveness and reversibility through a solvent injection (Sharma et al., 2019). Researchers are also exploring sperm motility inhibitors and gene-editing technologies as future options (Garcia and Matzuk, 2024). These advancements aim to provide reliable and reversible contraception for men, expanding birth control choices. Ongoing research and clinical trials are crucial to ensuring safety, effectiveness, and widespread accessibility.
The Demand for Male Birth Control
The demand for male contraception is growing. Studies suggest that many men are willing to use contraceptives if reliable options exist. Reducing unintended pregnancies can lower maternal health risks and alleviate financial burdens. Additionally, male birth control could contribute to decreasing abortion rates, particularly in regions with restrictive reproductive laws (Nguyen, 2024). ‘Despite well over half a century of effort in developing male contraceptives, there are no approved male contraceptive drugs on the market’ (Nickels and Yan, 2024).
The need for male contraception is urgent, especially in regions with high unmet contraceptive needs like Sub-Saharan Africa. In countries such as Burkina Faso and Uganda, both men and women show strong support for new male contraceptive methods. Introducing male contraceptives in these areas would ease the family planning burden on women, give men more control over their fertility, and promote gender equality (Cartwright et al., 2020). A study of 3,340 respondents in the U.S. suggests that 7–15.5 million men could be open to using novel male contraceptives (Nguyen, 2024). We can start by focusing on regions with high contraceptive gaps and working to raise awareness globally, pushing for public subsidies and support for research to drive progress (Nieschlag & Nieschlag, 2022).
Challenges and Barriers
Despite progress in developing male contraception, several challenges hinder its adoption. Societal norms often place reproductive responsibility on women, creating a barrier to behavior change (Preethy et al., 2022). Pharmaceutical companies are hesitant to invest in male birth control owing to concerns about market demand and potential profitability. Additionally, side effects and long-term safety remain significant issues that require further research. Overcoming these obstacles is essential for making male contraception a reliable and accessible option, providing men with more control over reproductive health while balancing societal expectations.
Addressing Gender Inequality in Reproductive Health
Contraception should not solely be a woman’s responsibility. Expanding male birth control options promotes shared responsibility, reducing the burden on women. By involving men in reproductive decision-making, relationships become more equitable. This shift can also empower women to make informed choices without pressure or fear of unintended pregnancy (Laurie et al., 2019).
The Future of Male Birth Control
Ongoing research continues to explore innovative male contraceptive methods. Clinical trials for new hormonal and non-hormonal options are advancing. Public awareness and policy support will play a crucial role in accelerating availability. Encouraging pharmaceutical investment and fostering societal acceptance are essential in making male contraception a viable and accessible option (Page et al., 2022).
Conclusion and Call to Action (CTA)
Male birth control represents a groundbreaking development in reproductive health. It offers the potential to reduce unintended pregnancies, decrease the transmission of STIs and HIV, and foster gender equity (Mags et al., 2020). Expanding male contraceptive options could relieve financial and healthcare burdens, enhance family planning efforts, and contribute to the achievement of SDG3: Good Health and Well-Being. Ensuring that male contraception is accessible, affordable, and widely accepted is not only a scientific challenge but also a critical global health necessity.
To successfully integrate male contraception into global health policies, governments and health organisations must increase investment in research and clinical trials for male contraceptives. Family planning programs should expand to include education on male contraception, ensuring that these options are affordable and easily accessible. Public awareness campaigns are vital for educating men about available contraceptive choices, while pharmaceutical incentives should be introduced to drive private-sector investment in the development of male birth control. By taking these steps, we can create a more equitable, healthier, and sustainable future for all.
Achieving THRIVE Project themes and the UN’s SDGs
Expanding male birth control aligns with multiple Sustainable Development Goals (SDGs). It directly contributes to SDG3: Good Health and Well-Being, reducing maternal mortality and improving reproductive health. Additionally, it supports SDG5: Gender Equality, by promoting shared responsibility in family planning, easing the burden on women, and fostering gender equity. The introduction of male contraceptive options also helps address SDG1: No Poverty, as it enables families to manage resources more effectively, avoiding the financial strain of unplanned pregnancies. Furthermore, it aligns with SDG10: Reduced Inequality, by improving access to reproductive health for marginalised groups, reducing health disparities, and ensuring better health outcomes for all.
A Thrivable Framework
It is beneficial to view male birth control through the lens of THRIVE’s Foundational Focus Factors (FFFs). Addressing Complex Wicked Problems, such as unintended pregnancies and gender inequality, requires applying Systems Thinking to address social, economic, and health challenges holistically. With the world’s resources under strain, it acknowledges Finite Resources, helping to reduce healthcare costs and ease the environmental pressures of rapid population growth. Built on Science-Based Targets, ongoing research ensures that male contraceptives are safe, effective, and reversible. By embracing Context-Based Metrics, these advancements are designed to meet real-world needs while considering broader societal impacts. Through a Multi-Capital approach, male contraception enhances economic, social, and environmental well-being, contributing to a Regenerative Economy that fosters long-term health, stability, and shared responsibility.
To learn more about our work, visit our website and explore how we’re making a difference. You can also follow our informative blog and podcast series, where you can dive deeper into the latest sustainability topics. Join our live webinars, where expert guests from various fields share valuable insights and answer your questions in real time. Sign up for our newsletter to stay up-to-date with upcoming events, fresh content, and exclusive opportunities.