WHAT IS UNIVERSAL HEALTH COVERAGE?
Universal health coverage (UHC) is defined by the World Health Organisation (WHO) as “ensuring that all people have access to needed health services of sufficient quality to be effective, while also ensuring that the use of these services does not expose the user to financial hardship” (2020).
UHC includes the full spectrum of essential, high quality health services, from health promotion to prevention, treatment, rehabilitation, and palliative care (WHO, 2019). It addresses the most significant causes of disease and death, ensuring everyone has access to services that will improve their health and prevent further illness. However, not all countries have universal health coverage.
SDG3: GOOD HEALTH AND WELL-BEING
As one of the targets of the SDG3 is achieving UHC, the World Health Organisation has prioritised it as a goal for health reform in many countries (2020). Countries that progress towards this will advance in other health-related targets and goals. The flow-on effect of good health includes an escape from poverty, a chance at a good education or job, and a basis for long-term economic developments (WHO, 2019).
THE BENEFITS OF UHC
The main benefit of UHC is that everyone can access good health care when and where they need it, which leads to a healthier nation and a reduced number of health-related deaths (Victor Kiprop, 2018). Importantly, the system also promotes equality as everyone receives the same treatment, no matter their age, gender identity, race, religion or financial situation.
Here are a few of the advantages of UHC (Kimberly Amadeo, 2020):
- Lowers overall health care costs: The government controls the prices through regulation.
- Lowers administrative costs: Doctors only have to deal with one government agency.
- Standardises services: Health care is not a competition or a way to make a profit. Hospitals and doctors provide the same standard of service at a low cost.
- Creates a healthier workforce: Preventive care reduces the need for expensive emergency room usage, allowing the space for patients in actual health emergencies to be treated quickly.
- Early childhood care prevents future social costs: Health education teaches families how to make healthy lifestyle choices, preventing health issues in the future which would put a strain on the health care system.
- Governments can guide the population toward healthier choices: By imposing regulations and taxes on drugs, cigarettes and alcohol, people are encouraged to make healthier decisions.
COUNTRIES WITH/WITHOUT UHC
Currently, approximately half of the world’s population do not receive the health services they desperately need (WHO, 2020). The majority of these people live in countries with no UHC system in place. The lack of affordable medical aid pushes 100 million people into extreme poverty each year because of out-of-pocket expenses (WHO, 2020).
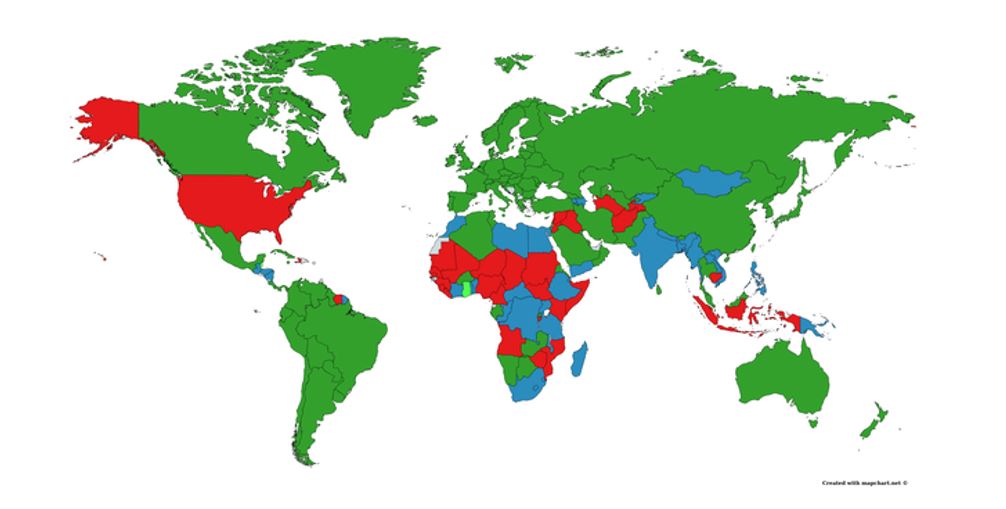
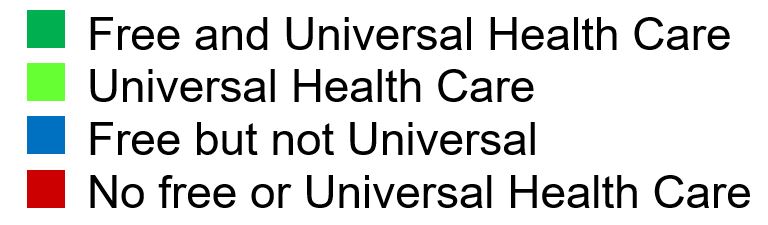
One of the most striking countries that do not have UHC is the United States. It is the only first world country to not have an established public health care system. The repercussions can be seen by comparing multiple factors, such as the cost of health care. In 2018, US health care cost 16.9% of GDP and despite this cost, the quality of care in some areas is worse than comparable developed countries (Kimberly Amadeo, 2020). The infant mortality rate was 5.6%, almost double that of Australia and Germany (Kimberly Amadeo, 2020). These statistics show the risks of not having UHC.
UHC AND COVID-19
The COVID-19 pandemic has placed enormous strain on countries around the world and has highlighted the importance of primary health care providers in responding to a global health crisis. Access to medicine and COVID-19 vaccinations at the community level has proved a much more efficient and effective approach to outbreak control than requiring people to travel to distant hospitals, potentially spreading the virus (Katherine Bliss, 2020). To reduce movement of people, health practitioners have increased the use of telemedicine for routine checkups (Katherine Bliss, 2020). Still, there are some who are unwilling to visit clinics at all in fear of contracting the virus.
The creation of new COVID-19 vaccines have had varied responses. For some it has brought hope, while others view their effectiveness with skepticism or feel scared. Therefore, it is important that health care providers build a trusting relationship with communities and share the necessary information to help patients make informed decisions about the vaccinations within the context of their overall health care (Katherine Bliss, 2020). By delivering high-quality care at the local level, health care facilities can roll out routine vaccination programs as well as mental health care services (Katherine Bliss, 2020).
HEALTH CARE FOR ALL
Improving health care services also depends on the ability of health care workers to deliver high quality care. Investing in the workforce, adequate supply of medicines, updating technologies and up-to-date education programs are some of the most cost-effective ways to ensure access to essential health care (WHO, 2019). UHC should also be based on a strong community-based health care, which not only focuses on preventing and treating illness but also on helping in improving the well-being and quality of life of the people (WHO, 2020). To make healthcare accessible to all, we will need to focus on the key aspects of community health.
LOOKING AFTER THE COMMUNITIES AND YOURSELF
Numerous countries are already making progress towards UHC. Moving towards UHC requires policy-makers to commit to investing in a strong health care system and render it as an affordable public service for anyone to access (WHO, 2020). THRIVE believes that by progressing towards UHC and SDG3, countries will become healthier and move towards sustainability. You may be thinking, as an individual, what can you do to improve the health of your community? By looking after your own health, you can help others do the same, especially during a global pandemic.
REFERENCES
World Health Organisation [WHO] (2020). Universal Health Coverage. Retrieved from https://www.who.int/healthsystems/universal_health_coverage/en/
World Health Organisation [WHO] (2019).Universal health coverage (UHC). Retrieved from https://www.who.int/news-room/fact-sheets/detail/universal-health-coverage-%28uhc%29
Kimberly Amadeo (2020). Universal Health Care in Different Countries, Pros and Cons of Each. Retrieved from https://www.thebalance.com/universal-health-care-4156211
Victor Kiprop (2018). Countries With Universal Health Care. Retrieved from https://www.worldatlas.com/articles/countries-with-universal-health-care.html
Katherine Bliss (2020). Universal Health Coverage and Primary Health Care within the Covid-19 Context. Retrieved from. https://www.csis.org/analysis/universal-health-coverage-and-primary-health-care-within-covid-19-context