Climate change is not a distant threat, it has become a health emergency affecting communities worldwide. Experts now call climate change ‘the biggest global health threat of the 21st century’ (Romanello et al., 2024), meaning that rising temperatures, shifting weather patterns, and more extreme events are already harming human health. From heatwaves that claim lives to storms that damage hospitals, the impacts are wide-ranging and urgent. In this article, we explore how climate change affects health, both physical and mental, and how healthcare systems can adapt to become more resilient.
Climate Change and Health
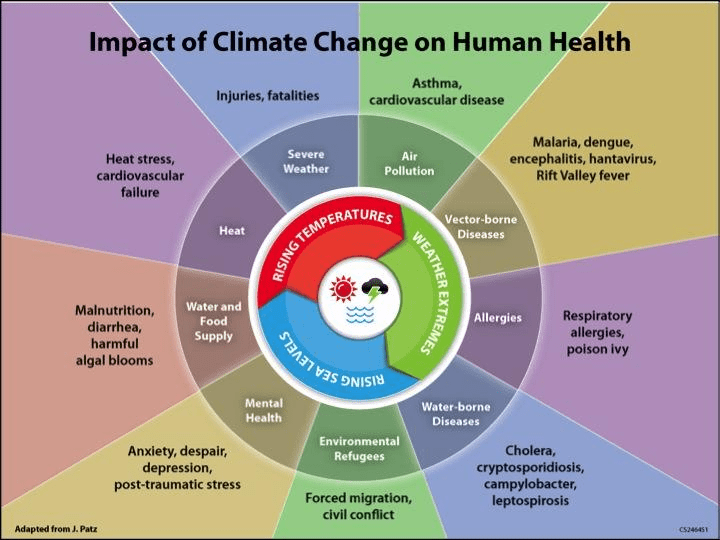
Climate change affects health through multiple pathways. It causes direct impacts – for example, extreme heat, storms, and floods can lead to injuries or death – and indirect impacts by altering our environment in ways that influence health. For instance, a warmer, wetter climate can increase the number of disease-carrying mosquitoes, worsen air pollution, and threaten food and water supplies. In short, climate change can make people sick or injured not only through immediate disasters but also through long-term shifts that increase disease and hardship (PAHO, n.d).
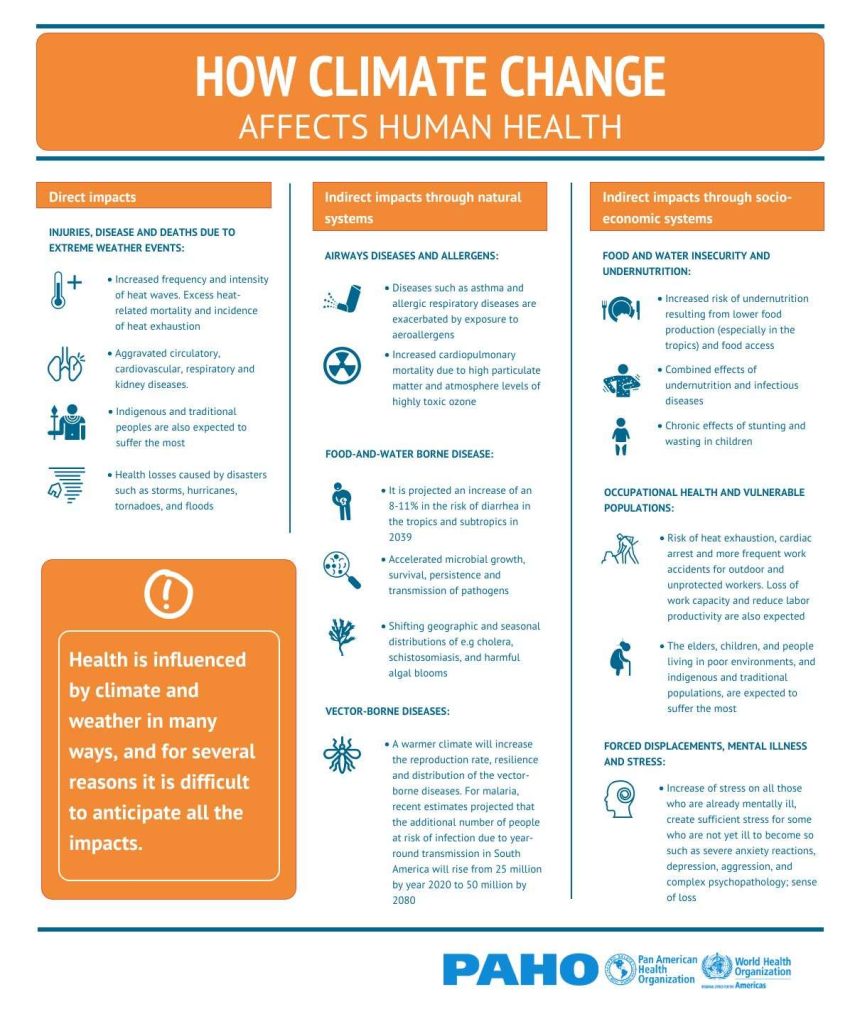
Source: PAHO, n.d
How Climate Change Affects Physical Health
Climate change is already harming physical health in numerous ways. Below are some major health problems linked to climate shifts—from heat-related illnesses to infectious diseases—and how certain populations are especially vulnerable.
Heat-Related Illnesses and Death
One of the clearest effects of a warming climate is the increase in extreme heat events. Heatwaves are becoming more frequent and intense, leading to more cases of heat exhaustion, heat stroke, and dehydration. Heat stress is already the leading cause of weather-related deaths in many regions (WHO, 2024).
High temperatures are especially dangerous for older people, outdoor workers, and people with chronic illnesses like heart disease or asthma. We have seen devastating examples: the 2003 European heatwave caused about 70,000 deaths (WHO, 2024). Between 2000-2019, globally, nearly half a million people died each year from heat exposure, and heat-related mortality in seniors has surged in the last two decades (WHO, 2024). The good news is that most heat-related illnesses and deaths are preventable. Simple public health measures, such as early warning systems for heatwaves, setting up cooling centres in cities, and checking on vulnerable neighbours, can save lives when implemented widely.
Worsening Air Quality and Respiratory Diseases
Climate change also dirties the air we breathe, worsening respiratory problems. Higher temperatures can boost the formation of ground-level ozone (smog), a lung irritant that triggers asthma, and other respiratory illnesses. Hotter, drier conditions also lead to more frequent wildfires, which fill the air with smoke and fine particles that can lodge deep in the lungs. Even people far from fire zones can experience coughs, bronchitis, or asthma attacks from drifting wildfire smoke (WHO, 2017).
Allergy seasons are also growing longer and more intense as warmer weather causes plants to produce more pollen, aggravating asthma and hay fever. These factors add up to a heavier burden of respiratory disease under climate change. Children, the elderly, and those with asthma or chronic lung disease are the most vulnerable to polluted or pollen-laden air. Notably, extreme heat and air pollution often go hand-in-hand; during heatwaves, stagnant air can cause pollution levels to spike, compounding health risks (WHO, 2017).
Spread of Infections and Vector-Borne Diseases
Changes in temperature and rainfall patterns are influencing the spread of infectious diseases. Warmer climates and altered rainfall expand the habitats of mosquitoes, ticks, and other vectors, meaning diseases like malaria, dengue fever, Zika, and Lyme disease are appearing in new areas that were previously too cool for these insects. Health experts report that illnesses such as malaria and dengue are already rising in higher altitudes and latitudes as the climate shifts (Lugten & Hariharan, 2022).
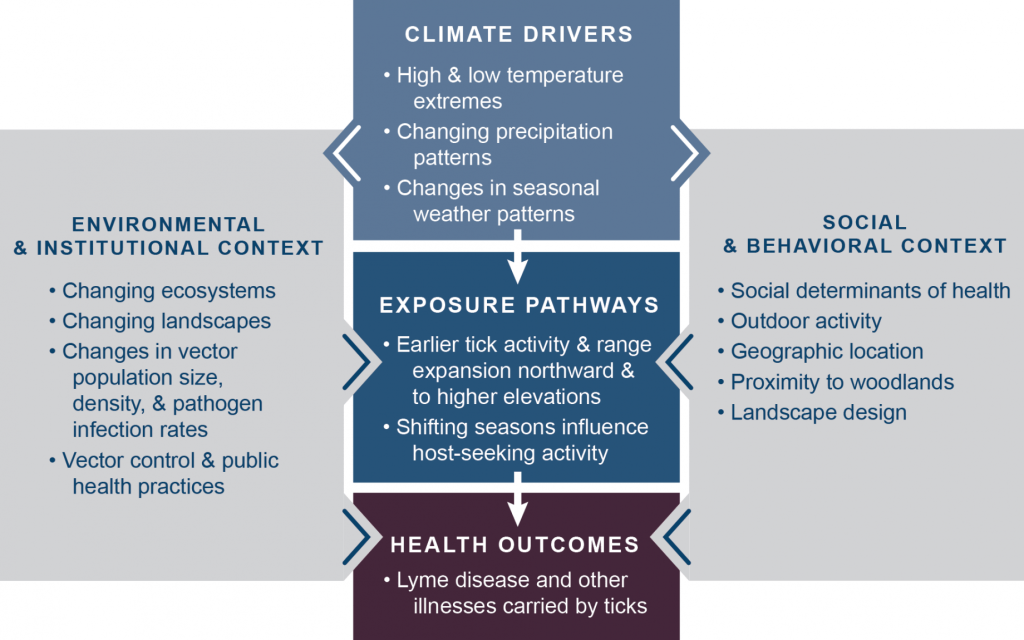
Source: GlobalChange.gov, 2016
Similarly, heavy rainfall and flooding can contaminate water supplies and lead to outbreaks of diarrheal diseases like cholera. Many of these diseases are highly climate-sensitive, and small environmental changes can greatly alter their spread. For example, dengue-carrying mosquitoes thrive in hotter, wetter conditions, so more regions with warming climates are seeing dengue outbreaks. Changing freshwater temperatures are also leading to increasing pathogens and bacteria that are harmful to human health. This means health authorities must closely watch disease patterns, gather data, and strengthen basic preventive measures (e.g. mosquito control, vaccination, water testing, and sanitation) to protect communities (WHO, 2017).
Vulnerable Populations at Higher Risk
Importantly, climate change does not affect everyone equally – some groups are far more vulnerable. The very young and the very old are at higher risk because of their fragile physical condition and dependence on others. People with chronic illnesses or disabilities also face greater dangers during events like heatwaves or evacuations. The economically disadvantaged and marginalised have the fewest resources: they often live in high-risk areas (e.g. flood zones or urban heat islands) and may lack sturdy housing, air conditioning, or access to medical care. Climate change can also worsen existing health inequities; those who contributed least to the problem (like low-income communities) often suffer first and worst. Protecting vulnerable populations will require targeted efforts to build resilience and ensure equitable access to resources in a changing climate.
How Climate Change Affects Mental Health
Beyond the visible physical illnesses, climate change is also taking a toll on mental health. It’s normal for people to experience stress, anxiety, grief, or even trauma in the face of a changing environment and more frequent disasters. These psychological impacts may be less obvious but are very real.
Eco-Anxiety and Climate Grief
Many people, especially young people, are feeling anxious about climate change and the future of the planet. Psychologists refer to this as “eco-anxiety,” meaning a chronic fear about climate change. Surveys show that a majority of adults now feel some level of eco-anxiety about climate change (APA, 2020).
This anxiety can range from a general worry to, in some cases, more severe distress or insomnia about what climate change means for our collective future. Closely related is climate grief (or ecological grief), feelings of sadness and mourning as people witness the loss of ecosystems, wildlife, and landscapes (Comtesse et al., 2021). For example, seeing a beloved forest devastated by wildfires or coral reefs dying can provoke grief similar to losing a loved one. While some level of concern is normal and can motivate action, intense eco-anxiety or climate grief can become overwhelming and interfere with daily life.
Trauma and Stress from Disasters and Displacement
As climate-related disasters (hurricanes, wildfires, floods, etc.) increase, so do cases of trauma and chronic stress. Surviving a life-threatening event can lead to post-traumatic stress disorder (PTSD), depression, or anxiety. People may lose their homes or loved ones and face a long, difficult recovery, all of which strains mental well-being. The stress isn’t limited to the immediate aftermath – ongoing rebuilding and the fear of another disaster can keep anxiety high for years. Climate change is also forcing some communities to leave their homes entirely. Displacement owing to climate impacts, whether sudden (fleeing a wildfire) or gradual (relocating because of rising seas), is extremely stressful. Being uprooted, losing one’s community, and facing uncertainty in a new location can cause deep emotional distress. The World Bank projects that over 200 million people could be internally displaced by climate change by 2050 (World Bank, 2021).
Families who are displaced often experience grief for what they left behind and anxiety about the future. All of this contributes to the psychological toll of climate change. It highlights the need to include mental health support in disaster response plans, for example, providing counseling and community programmes after traumatic events (Lugten & Hariharan, 2022).
Source: GenEngNews
Adapting Healthcare Systems to a Changing Climate
With climate change already unfolding, healthcare systems must adapt to protect public health. Just as we reinforce buildings against earthquakes, we need to climate-proof our hospitals, clinics, and public health services. A top priority is strengthening healthcare infrastructure. Hospitals and clinics should be designed or retrofitted to withstand extreme events, for example, ensuring they have backup power during heatwaves or storms, flood defences where needed, and ventilation systems that can handle extreme heat or wildfire smoke. However, in the Americas, about 67% of hospitals are located in disaster-prone areas, and in the past decade, millions of people lost access to care for months because healthcare structures were damaged by disasters (PAHO, n.d).
Another key focus is emergency preparedness and planning. Health systems need robust plans for responding to climate-related events and emerging health threats. This means training healthcare staff to recognise and treat illnesses like heat stroke or smoke inhalation. This also means stockpiling essential supplies and coordinating with emergency services for disasters. Early warning systems can be integrated so hospitals and communities can be prepared for increased climate-dependent illnesses (PAHO, n.d).
Policies and investments should support these efforts. For example, creating heat action plans for cities, improving disease surveillance for climate-sensitive illnesses, and incorporating health into national climate adaptation plans. Strengthening healthcare in this holistic way will help ensure that our health systems remain reliable and effective in a changing climate.
The Urgency of Adaptation and Mitigation
Time is of the essence. Every action we take towards building resilience now, can translate into lives saved in the future. The health impacts we’re witnessing, from wildfire smoke choking cities to the rise in climate anxiety, will only worsen if we delay. But if we act boldly, we can create a healthier, safer world for ourselves and future generations. Climate change is not just an environmental issue but a fundamental public health challenge that demands urgent attention.
We need both adaptation (to protect ourselves from current and future impacts) and mitigation (to reduce greenhouse gas emissions and limit future warming). Without cutting emissions, adaptation efforts could be overwhelmed; without adaptation, changes already set in motion will take an unnecessary toll on lives.
The THRIVE Framework
Tackling climate change’s health impacts requires a systemic, values-driven healthcare transformation that integrates Values-Based Innovation, Systems Thinking, and a Regenerative Economy, three key Foundational Focus Factors of the THRIVE Framework.
Values-Based Innovation shifts healthcare from a profit-driven model to one that prioritises well-being, sustainability, and social equity. This means focusing on preventative care, climate-smart hospitals, and digital health solutions that improve access while reducing emissions. Instead of emphasising efficiency or cost-cutting, healthcare systems must integrate sustainability, ethical technology, and planetary health to ensure long-term resilience and health security.
Systems Thinking highlights the deep connection between human and planetary health. Climate change is more than an environmental crisis, it is also a health crisis driven by pollution, food systems, urban planning, and healthcare infrastructure. Health policies must address these interdependencies to build climate resilience. For example, reducing air pollution slows global warming while also preventing respiratory diseases and cutting healthcare costs. This demonstrates the power of a holistic, cross-sectoral approach.
A Regenerative Economy goes further by urging healthcare systems to restore and replenish the natural and social systems they rely on. Moving beyond sustainability, regenerative models ensure that hospitals and clinics reduce waste, use renewable energy, and support local economies. They also promote social equity in healthcare access. By adopting a circular, restorative approach, the healthcare sector can lower its climate footprint while actively repairing environmental damage.
Conclusion
These efforts align with the United Nations Sustainable Development Goals, especially SDG13: Climate Action, which emphasises the urgent need for countries to strengthen adaptive capacity, mitigate climate impacts, and enhance resilience against environmental disruptions (UN, n.d).
SDG13 highlights how closely human health and well-being depend on addressing climate vulnerabilities through proactive, coordinated strategies. Furthermore, this approach directly supports SDG3: Good Health and Well-Being, recognising the intrinsic connection between a stable climate and the overall health outcomes of populations globally.
Additionally, incorporating Values-Based Innovation contributes to SDG10: Reduced Inequalities by ensuring climate adaptation strategies are equitable and inclusive, protecting the most vulnerable communities. Systems Thinking, another Foundational Focus Factor of the THRIVE Framework, emphasises the need to consider systemic properties to tackle planetary emergencies. We need to take into account all the interconnected ways in which climate change can impact the world and all living beings. By synergising these sustainable development goals and the THRIVE Framework, we can meaningfully tackle climate-related health challenges, driving a comprehensive, equitable, and resilient transformation benefiting both people and the planet.
At THRIVE, we envision a future where sustainability and healthcare represent not an endpoint but a starting point for transformative change. Through research, education, and advocacy, we explore pathways that extend beyond sustainability toward thriving systems. Engage with our blogs, podcasts, and webinars featuring fresh perspectives from leading experts, and subscribe to our newsletter for timely updates on systemic innovation and regenerative solutions. Join our community and help drive the transition to a future where humanity and the planet flourish together—a truly thrivable future.